Stop the Pain: 3 Exercises to Fix Badminton Knee & Recover Faster
Knee pain shouldn’t end your badminton journey. ST Badminton Academy shares the “Active Rehab” framework used by sports physios to treat patellar tendonitis (“jumper’s knee”) and anterior knee pain. Whether you play in Kepong, Setapak, or Wangsa Maju, this guide teaches you how to manage load, strengthen the tendon safely, and return to the court without relying solely on painkillers or indefinite rest. Note: This is educational guidance, not a medical diagnosis.

1.1 Why It Hurts
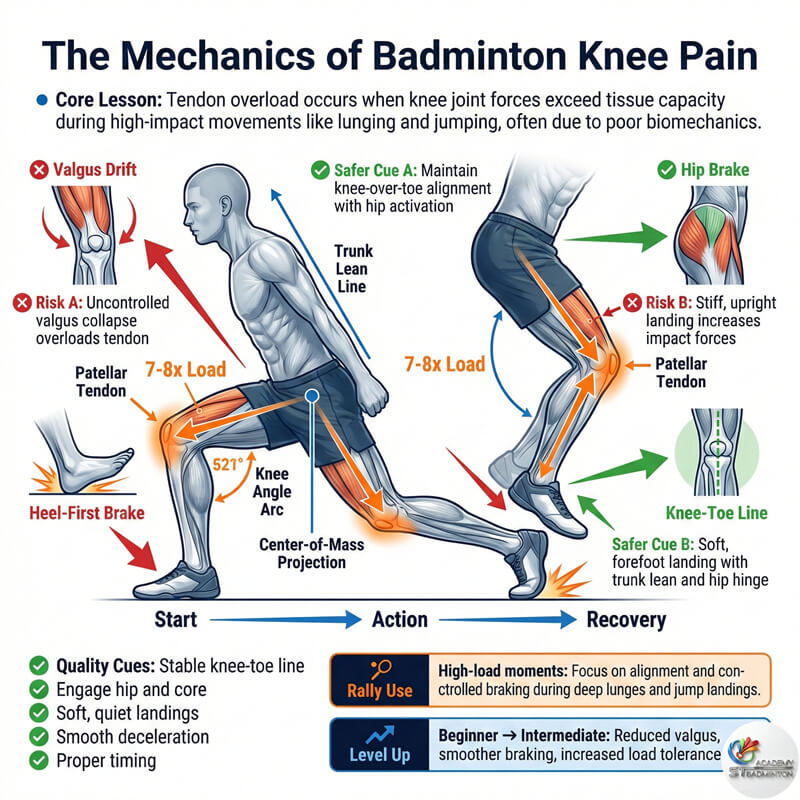
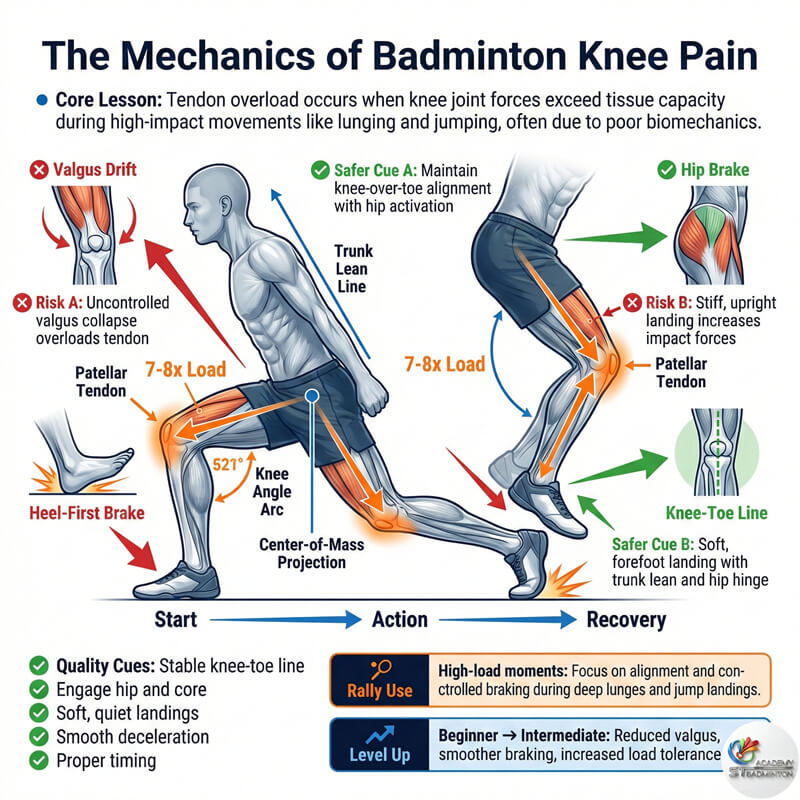
The Mechanics of Badminton Knee Pain
Knee pain in badminton typically stems from Load Capacity failure. Every time you lunge deep or land from a jump smash, your patellar tendon absorbs force up to 7-8 times your body weight. If you increase training intensity too fast or if your glutes and quads aren’t strong enough to act as “brakes” the tendon gets overloaded and irritated.
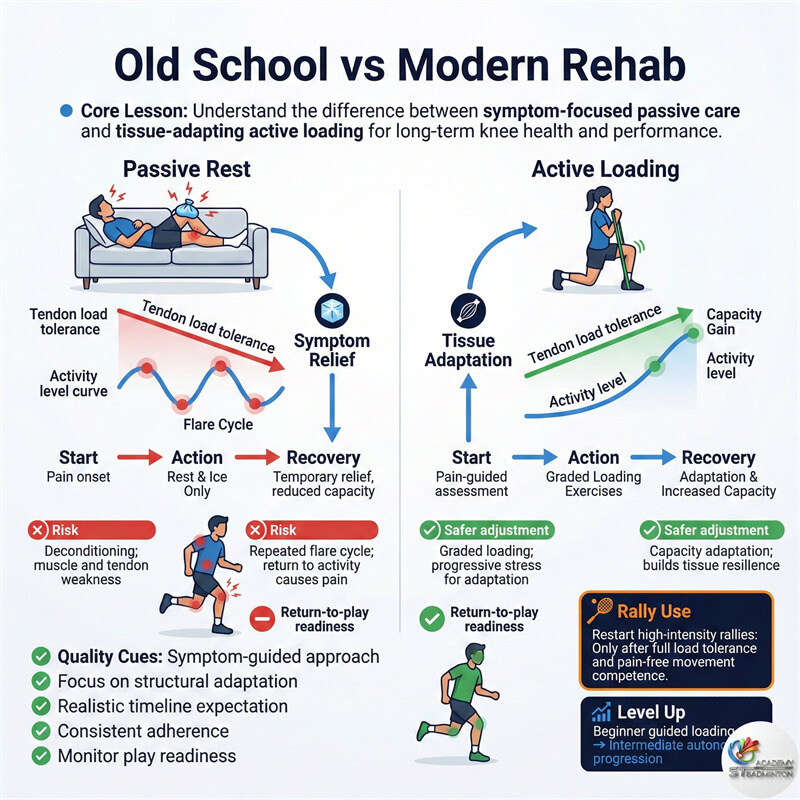
This is commonly known as patellar tendinopathy. The pain is usually right below the kneecap. The mistake most Malaysian players make is either resting completely (which weakens the tendon further) or pushing through the pain (which causes damage).
The solution lies in the middle: Active Recovery. You must stop the aggravating movements (jumping) and replace them with safe loading exercises to rebuild the tendon’s strength.
Exercise 1: The Painkiller
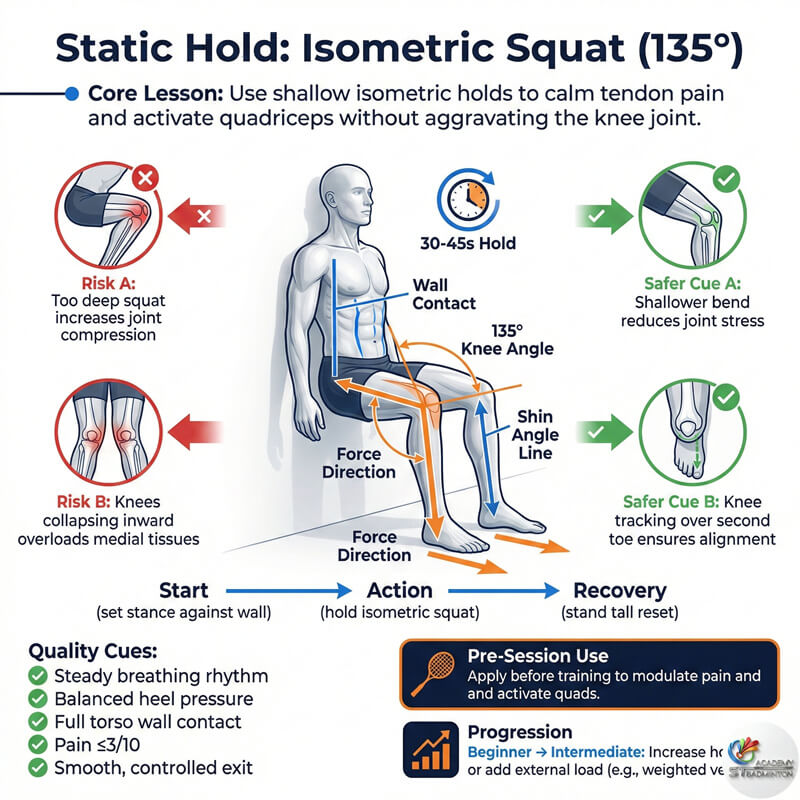
Static Hold: Isometric Squat (135°)
Isometrics (holding still under load) are magical for tendon pain. They reduce pain perception immediately while keeping the muscle active. We recommend the “135-degree Wall Sit.”
How to do it: Lean against a wall and slide down until your knees are bent at about 45 degrees (a shallow squat, not a deep 90-degree sit). Your shin should not be vertical; feet should be slightly forward.
Dosage: Hold for 30 to 45 seconds. Rest for 2 minutes. Repeat 3-5 times. Do this daily or before training as a warm-up. This is often the first step we prescribe to students in our Gombak classes who complain of “warm-up pain.”
Exercise 2: The Decelerator
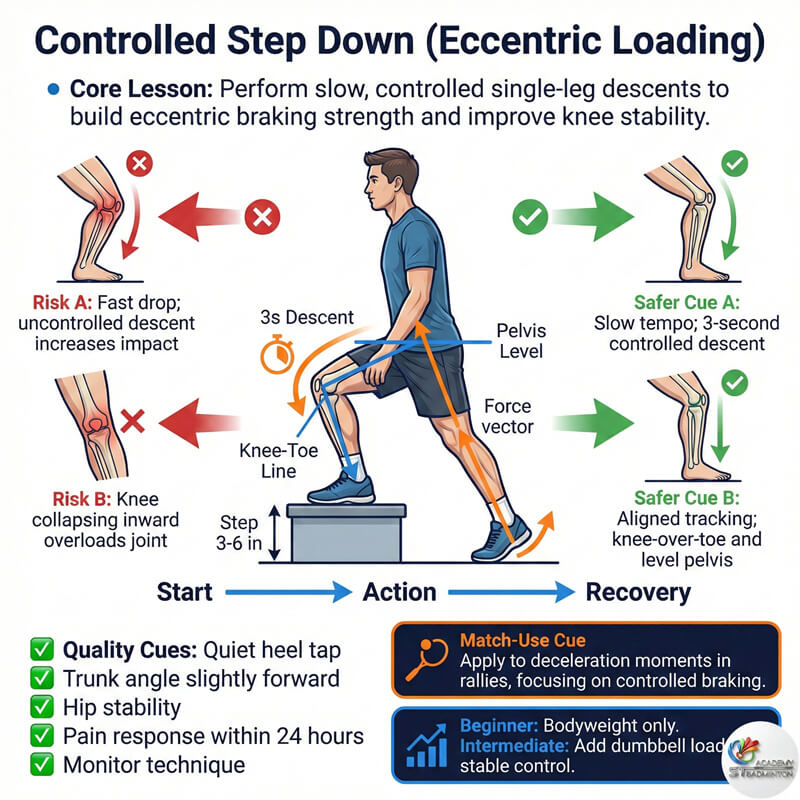
Controlled Step Down (Eccentric Loading)
Badminton is a sport of braking. Most pain occurs when you try to stop a movement (eccentric load). This exercise builds that specific braking strength.
How to do it: Stand on a low step or a thick book (approx 3-6 inches high). Slowly lower your non-injured leg to tap the floor with your heel, taking 3 full seconds to go down. Keep the knee of the standing leg aligned with your second toe do not let it collapse inward.
Progression: Start with bodyweight. Once pain-free, hold a water bottle or dumbbell. Aim for 3 sets of 10-12 slow reps. If pain exceeds a 3/10, lower the step height.
Exercise 3: The Lunge Fix
Split Stance Holds
Badminton requires lunging. To return to play safely, you must re-teach your tendon to handle the lunge position without irritation. The Split Stance Isometric is a safe way to simulate a lunge.
How to do it: Get into a stationary lunge position. Keep your front shin vertical (do not let the knee travel far past the toes yet). Your back knee hovers just above the ground. Hold this position statically.
Dosage: 30 seconds hold per leg, 3 sets. This builds quadriceps endurance in a position specific to badminton. As you get stronger, you can hold dumbbells.

1.5 Return to Play
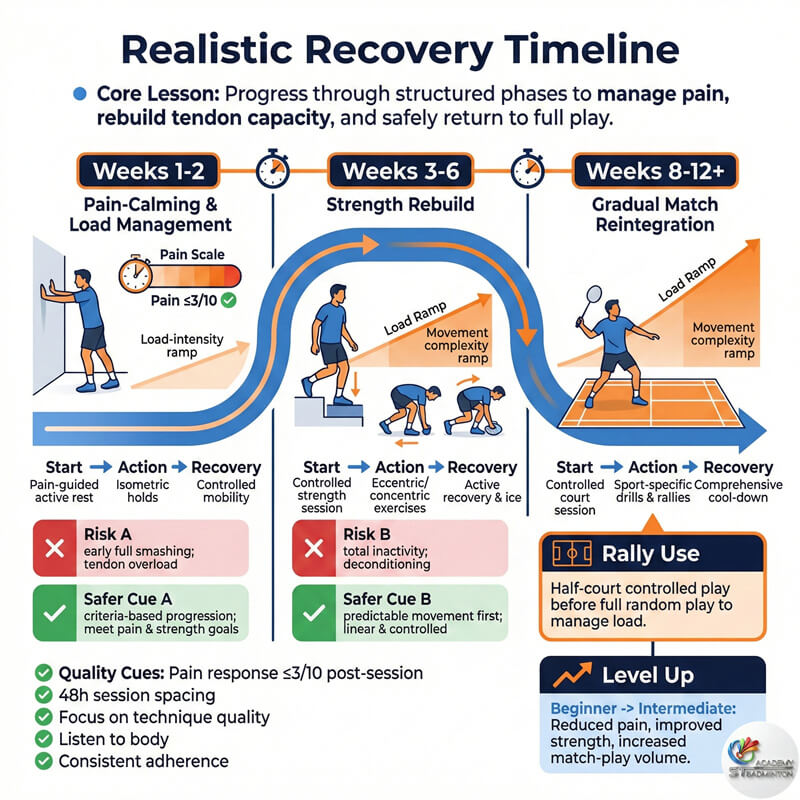
Realistic Timeline
Recovery is not a straight line. Here is a conservative timeline for typical jumper’s knee recovery, assuming you follow the exercises:
Weeks 1-2: Focus on pain management. Use Isometrics (Exercise 1) daily. Stop all jump smashing and deep lunging. Continue stationary shots.
Weeks 3-6: Introduce Eccentrics (Exercise 2) and Split Stance (Exercise 3). Return to light drilling (fixed footwork, no random jumping). Pain should be below 3/10.
Weeks 8-12+: Gradual return to match play. Start with half-court singles or doubles where movement is predictable. Full smashing capacity returns last.
1.6 Red Flags
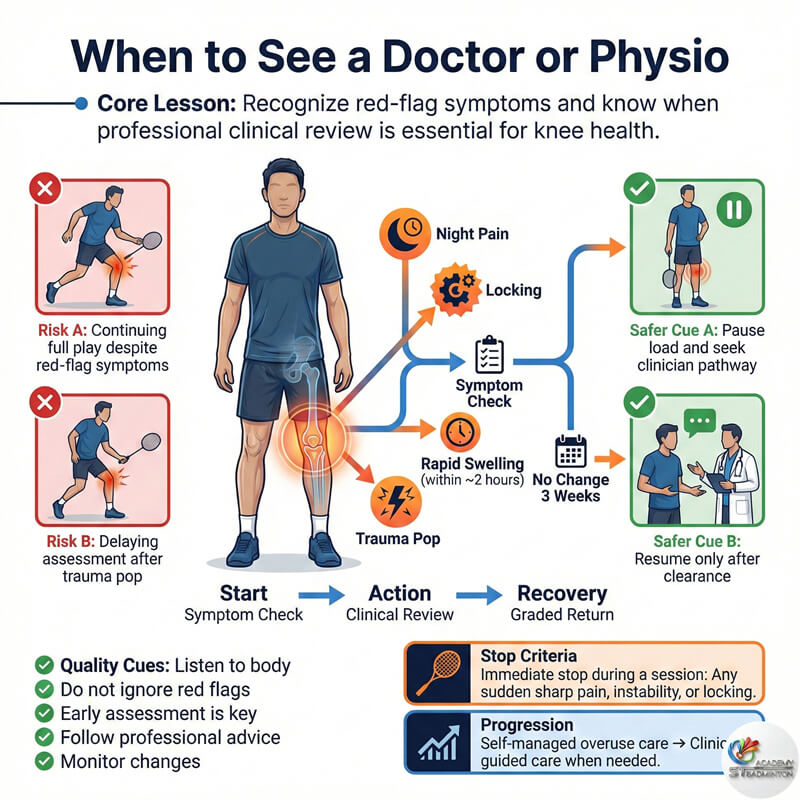
When to See a Doctor or Physio
While active recovery helps most overuse injuries, some symptoms require immediate professional attention in Malaysia (visit a sports clinic in KL or Selangor):
• Locking/Clicking: If your knee gets “stuck,” it could be a meniscus tear.
• Night Pain: Pain that wakes you up at night is a red flag.
• Immediate Swelling: If the knee swells up within 2 hours of injury (pop), suspect an ACL/ligament issue.
• No Improvement: If 3 weeks of load management and isometrics yield zero change.
1.7 Prevention Strategy
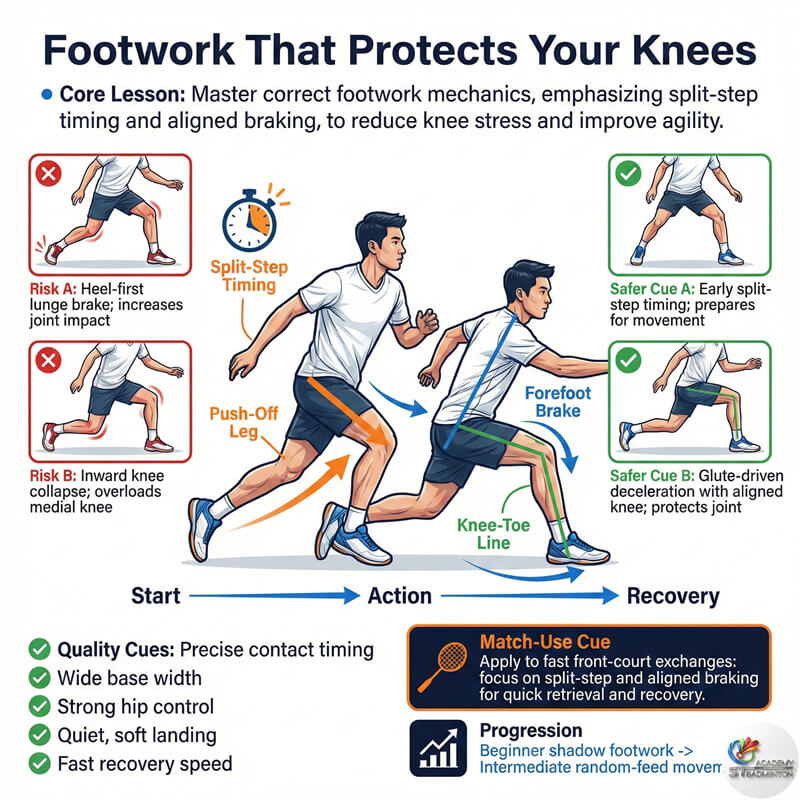
Fix Your Footwork to Save Your Knees
Once the pain subsides, you must address the root cause. For 80% of our students in Kepong, knee pain comes from “lazy footwork” landing with the heel first on lunges (braking too hard) or letting the knee collapse inward (valgus stress).
At ST Badminton Academy, we re-train your split step timing and lunge alignment. By using your glutes to decelerate rather than jamming your knees, you can play pain-free for years. Prevention is always better than rehab.
Knee Recovery FAQ (Malaysia Edition)
Practical answers on managing and recovering from badminton-related knee pain.
What is common badminton knee pain?
Usually Patellar Tendinopathy (Jumper’s Knee) or Patellofemoral Pain Syndrome (Runner’s Knee). It feels like a dull ache below or around the kneecap, worsening with jumping or deep lunges.
Is complete rest better?
No. Complete rest for tendons (unless acute rupture) makes them weaker. “Active Rest” is better reduce the load (stop jumping) but keep the tendon loaded with safe isometric exercises.
What is a 135° static squat?
It is a wall-sit where your knees are only slightly bent (about 45 degrees from straight). This position puts less stress on the kneecap while still activating the quad muscles to support the tendon.
How often should I do exercises?
Isometrics (Exercise 1) can be done daily, often 2-3 times a day for pain relief. Strength exercises (Exercise 2 & 3) are best done 3-4 times a week with rest days in between.
Can beginners use this plan?
Yes. These are foundational rehab exercises. Beginners usually benefit fastest because their pain often comes from lack of strength rather than chronic wear and tear.
How long until full recovery?
Mild cases often resolve in 3-6 weeks with diligent exercise. Chronic cases (pain for months) may take 12+ weeks to rebuild full load tolerance for competitive play.
What if pain increases?
Stop the exercise immediately. A little discomfort (3/10) is okay during rehab, but pain should settle within 24 hours. If it spikes and stays high, you are overloading. Rest and regress the exercise.
Ice or Active Rehab first?
Ice manages symptoms (pain relief) but does not fix the problem. Active rehab (loading) fixes the structure. Use ice only for acute flare-ups; prioritize active loading for long-term recovery.
When to see a doctor?
If you have night pain, locking, giving way, massive swelling, or if the pain was caused by a specific trauma event (like a twist or fall). These require a scan (MRI/X-ray).
Recovery & Rehab Gallery

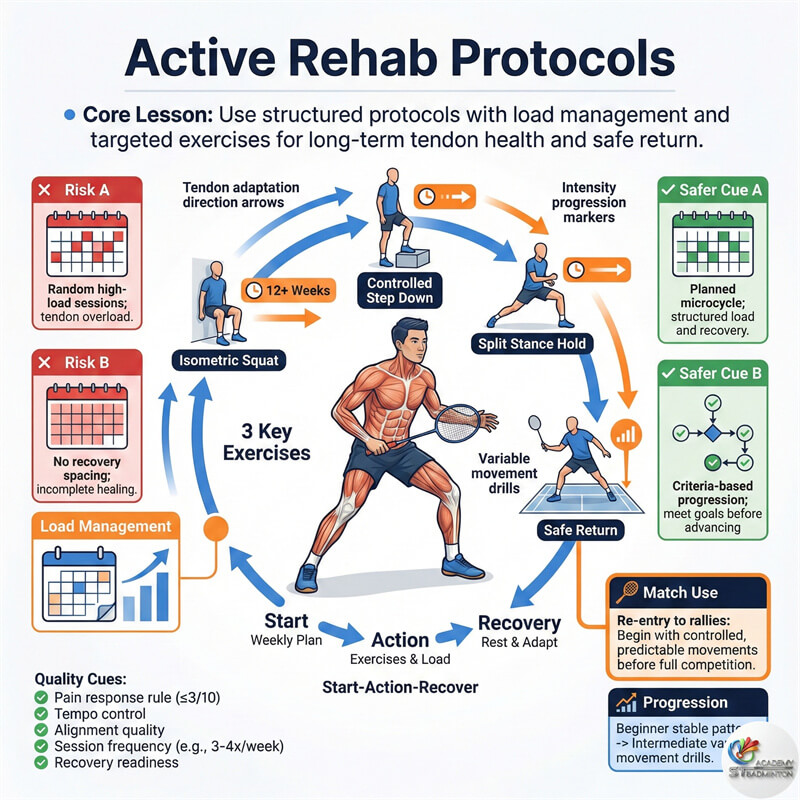
Rehab Protocols
We use modern, active recovery protocols to ensure tendons heal stronger, not just rest weaker.
| Feature | Passive Rest (R.I.C.E) | Active Rehab (Loading) |
|---|---|---|
| Goal | Symptom relief only (hide pain) | Tissue strength adaptation |
| Activity | Total inactivity (Ice & Rest) | Safe loading (Isometrics) |
| Result | Tendon weakens, pain returns on play | Tendon strengthens, capacity increases |
| Timeline | Uncertain (cycle of flares) | Progressive (weeks to months) |
| Best For | Acute trauma (first 48 hours) | Chronic overuse / Tendonitis |
Book a Rehab Consultation in Kepong
Don’t guess with your recovery. ST Badminton Academy works with sports science principles to help you return to play safely. Contact us to schedule a technique assessment or to discuss your return-to-play strategy with Coach Eric.